The Three Pillars
Progress towards UHC requires government action in three main areas:
Countries that have been successful in introducing national health systems have done so by pooling funds so that the cost of healthcare is shared more equally across society. This can be done by using income tax, or by asking every citizen to pay into a national insurance scheme according to how much they earn. Many countries provide free health care to those who are not earning, including children and young people, the elderly and those on low incomes. For example, Mexico has been able to move towards UHC by increasing government – or public – spending on health by an average of 5% annually from 2000 to 2006.
Domestic Health Financing Mechanisms
How do countries pay for healthcare? In countries with national health systems, this is done through taxation (for example, in Brazil, Thailand and the UK) or other government income (for example, in Bahrain, Kuwait and the UAE). However, many countries also have national health insurance schemes, whereby citizens pay an annual membership fee (for example, in Belgium and Ghana). Some countries, including Kenya and Tanzania, are considering innovative financing mechanisms. Botswana for example has used a tax on alcohol since 2008 to fund the Ministry of Health and other initiatives.
UHC is about more than financing. Health systems, including facilities, medicines, data systems, staff and volunteers need to be strengthened to ensure high-quality health services are available where they are needed. A renewed focus on service delivery through an integrated and people-centred lens is critical to reaching underserved and marginalised populations and promoting patient safety to ensure that everyone has access to the quality health services they need. Moreover, broadening the range of services to include health promotion, prevention, rehabilitation and palliative care is vitally important.
To achieve UHC, governments also need to promote different sectors to work together to address the non-medical causes of ill-health and disease, such as low education, conflict, discrimination and poverty. Research has shown that these factors (known as social determinants of health ) can be more important than health care or lifestyle choices in influencing health.
While health financing and service delivery are essential, health system governance is critical for success. Without good governance, UHC implementation can become narrowly defined, inequitable and ineffective. According to WHO, effective health governance requires the full engagement of three key stakeholders:
- The State (government organizations and agencies at central and district level)
- Health service providers (public and private, for and not for profit, clinical, para-medical and non-clinical health services providers; unions and other professional associations; networks of care or of services)
- The citizen (population representatives, patients’ associations, CSOs, NGOs, citizens associations protecting the poor, grassroots advocates, etc.)
Good governance involves dialogue between the government and its people, not only to build trust and enable effective implementation, but also to ensure that reforms are co-owned by populations, communities and civil society.
To achieve equitable policies for health, citizens’ voices must be strengthened and fostered with meaningful roles in decision-making. There must be policy and legal frameworks that protect against discriminated health service delivery, regulate the sector appropriately, and allow transparent governance. Lastly, it is important to develop coalition-building and opportunities for collective action and partnership.
The importance of civil society participation in UHC planning, implementation and monitoring is explored in more depth in Part Two: Why civil society should engage in UHC.
National health policies, strategies and plans (NHPSPs)
This is a generic term for the range of national government health policies, strategies and health plans that set out policy on health reform and UHC. NHPSPs ensure that countries allocate domestic resources efficiently and fairly, and that domestic budgeting for health is consistent and predictable.
Planning is often made into something complicated, a mystery wrapped in jargon, process and politics. Planning is sometimes left to the professional planners or the managers to control and do. That is a mistake. The best operational plans, and certainly the ones most likely to be implemented, are those that are developed with the people who will carry them out.”
– Strategizing National Health in the 21st Century: A Handbook
A UHC Partnership Resource, UHC Partnership
How UHC Works: Three Dimensions
WHO encourages national governments to see their health reforms as an ongoing journey—as steps contributing to continuous progress toward UHC.
One of the most helpful ways to think about governments’ strategic choices as they undertake this journey is the UHC Cube diagram in The World Health Report, 2010:
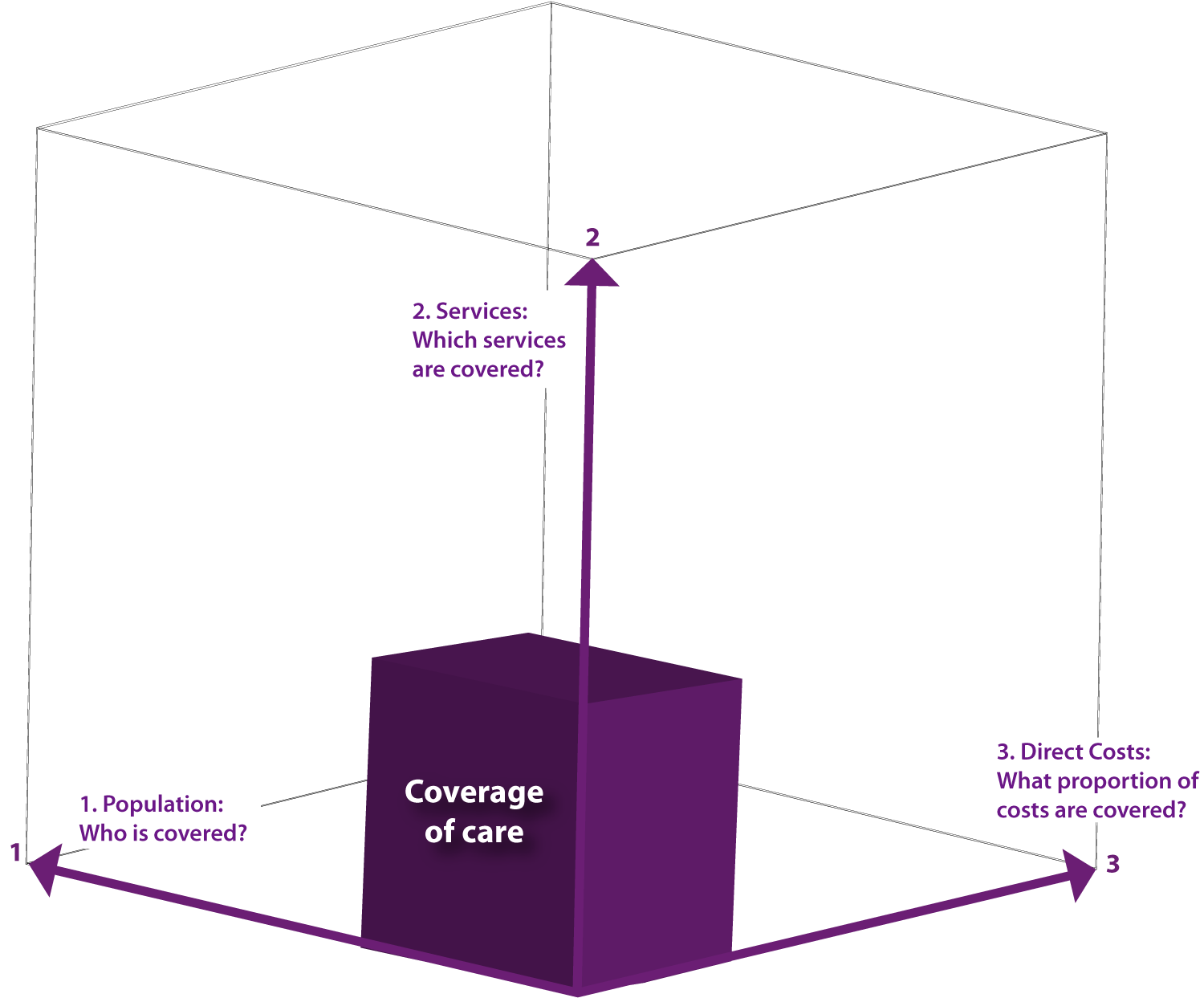
This diagram proposes that governments plan their UHC strategies taking into account the three key policy questions that make up the three dimensions of the cube:
- Who in the population is covered?
- What services are they covered by – and at what level of quality?
- What level of financial protection do citizens have when accessing services?
Health Benefit Package
The services that are to be covered by the government to make progress toward UHC are described as the ‘Health Benefit Package’. This is a core set of services that a government considers essential to meet the health needs of the population and for which they are willing to pay. Explicitly defining this package allows governments to cost and plan their budgets, and informs citizens of what is covered and importantly, where there are still gaps.
The content of the health benefit package should be informed by three considerations:
- Equity – ensuring equal and fair access to services
- Disease burden profile – the main health needs of the population
- Cost-effectiveness analysis – aiming to achieve the greatest impact given the available resources
Global Political Commitment
In 2015, all countries worldwide committed to achieving UHC by 2030 as part of the SDGs. It is a genuinely global goal in that there is scope for improvement in all countries, even where there is national health insurance or where health services are already provided free to all citizens.
Progress on this goal is measured by the size of the population covered by essential health services and the number of people who experience financial hardship from health costs. This global commitment was confirmed again in 2019 at the UN High-Level Meeting on UHC, with the resulting Political Declaration setting out the “most comprehensive set of health commitments ever adopted.”
In early 2019, diverse actors across the UHC movement – from parliamentarians and civil society to the private sector and academia – shared their calls to action for leaders ahead of the UN High-Level Meeting on Universal Health Coverage. This participatory process resulted in the Key Asks from the UHC Movement, which helped influence the commitments made in this political declaration. Learn more about the specific global commitments on UHC.

Primary Health Care
Primary health care (PHC) refers to basic health services provided at the community level. It includes a wide range of services, including vaccination, maternity and infant care, preventative and palliative care. Increased public investment in primary health care is one of the best ways to ensure equity, availability, accessibility, quality and efficiency of the health service.
UHC in the Sustainable Development Goals (SDGs)
SDG3: Good Health and Well-being: Ensure healthy lives and promote well-being for all at all ages
Target 3.8: Achieve universal health coverage, including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all.
- Indicator 1: Coverage of essential health services
- Indicator 2: Proportion of population with large household expenditures on health as a share of total household expenditure or income
Population
Who is covered?
Governments are encouraged to progressively expand coverage of health services to 100% of the population. This does not necessarily mean that services are free. In many wealthy countries, the only barrier is cost.; however, migrants, prisoners, rural populations, and indigenous people are just some groups that struggle to get access to health even in these settings. Currently, no country in the world has achieved this goal. Expanding government spending on health is important to ensure no one is left behind.
The question of who in the population receives financial protection is addressed through good governance, as discussed in the section above on the Governance pillar.
Services
What is covered?
The range of health services available in a country depends on many different factors. The US and Switzerland are known for having the top medical services in the world. Governments are encouraged to improve their domestic health services progressively, but these are limited to very basic medical care in many places.
The services covered financially by the government are described as ‘health benefit packages’. These should be informed by the evidence on ensuring equity, addressing health needs of the population and achieving the greatest impact with available resources.
According to WHO, the content of a health benefit package should be informed by three considerations:
- Equity—ensuring equal and fair access to services
- Disease burden profile—the main health needs of the population
- Cost-effectiveness analysis—aiming to achieve the greatest impact given the available resources.
Financial Protection
What do people have to pay?
Many countries request citizens pay a proportion of health-care costs from their own pocket, either through insurance premiums, co-payments or prescription charges. Governments are encouraged to progressively remove these out-of-pocket (OOP) payments in preference of general taxation, pooled funds and health levies on goods.
Some countries focus on financially covering the most vulnerable, for example, those on low incomes, children under five, and the elderly. For instance, in Senegal, the ‘Sesame Plan’ provides free health care to all those over the age of 60. However, in many countries, national health insurance is only available to those in formal employment or who have a family identification card.

