Civil society organizations and communities play a vital role in holding governments accountable for their UHC commitments, and ensuring that health policies and programs are inclusive, equitable and responsive to all. To that end, civil society actors convened by CSEM and partners developed the four advocacy messages below in the lead-up to the UN High-Level Meeting on UHC in 2019, complementing the specific commitment areas of the Key Asks from the UHC Movement.
These four messages were further tailored to civil society and community needs in 2020 through a consultative process to develop CSEM’s Calls to Action for COVID-19.
Below, read more about each advocacy message from civil society and why they are important to achieve for the COVID-19 response and beyond. Also included below are the Key Asks from the multi-stakeholder UHC movement, which we encourage you to incorporate into your advocacy efforts.
1: Leave No One Behind
SUMMARY: Civil society is often best placed to gain access to, represent, and prioritize the most marginalized key populations. To leave no one behind, civil society is a critical voice in ensuring that such people and communities:
- Are central to health reforms.
- Have the necessary access to equitable health services of good quality.
- Are informed of health policies and reforms.
- Can input into their country’s health systems strengthening efforts.
Health is a human right, and all countries have a duty to fulfil this right to health for all. Yet the current global reality is increasingly a lack of access to health for the most vulnerable. Globally, the poorest and most marginalized people bear the brunt of preventable mother and child deaths, heart disease, cancer and infectious diseases, such as COVID-19.
National health plans and policies, including those in response to COVID-19, need to assess which populations are currently left behind and have insufficient access to health services. They should identify scale-up plans for access, explicitly targeting those populations most in need.
Health data collection systems must be disaggregated (e.g. by sex, age, gender identity, ethnicity, disability and economic status), accompanied by robust monitoring and evaluation mechanisms that better inform and define the necessary policies. Civil society organizations, especially those serving and led by affected communities, are central to contributing this information using participatory data collection approaches.
Multidisciplinary approaches are needed that include sectors outside health (e.g. education, agriculture, environment, and economic development) to address the broader effects of the COVID-19 pandemic, such as food and water shortages, the increased risk of home-based violence against women and children, and increasing basic support for people with disabilities.
Community-owned and led health services can also play a vital role in providing expanded health coverage to the poorest and most marginalized groups.
How have CSOs responded to COVID-19 so that no one is left behind?
CSOs are working to ensure that the COVID-19 response protects everyone and the momentum for UHC is maintained amid the crisis. Civil society organizations have been actively engaged in their communities, providing critical services at the frontline and protecting those bearing the brunt of the pandemic. Civil society organizations have been resilient and creative in responding to the challenges of COVID-19 and related lockdowns and disruptions—often without any institutional support—and at the same time continuing the fight for UHC. They have also advocated governments to prioritize marginalized groups, including people with disabilities, so they are given precedence in vaccination and other essential support systems during the pandemic.
The best way to ensure that the voices of vulnerable groups with specific needs or additional risks are represented is to engage civil society in both short and long-term COVID-19 decision-making processes and task forces. Civil society understands and can advocate recognizing that different groups have different needs and constraints that require adapted solutions.
2: Increase Public Financing for Health
SUMMARY: Civil society can mobilize a broad-based advocacy movement to demand greater government investment in health to reduce reliance on foreign aid. Most countries—even those with the least resources—can mobilize the necessary funds to progress towards UHC.
Despite economic growth in many countries, domestic funding for health has failed to keep pace, with many governments continuing to rely on external health aid. However, lack of investment in UHC at a national level threatens global health security—as we have seen with COVID-19.
All UHC plans need to include specific action points to abolish user fees and direct patient payments to reduce and eventually eliminate OOP expenses. Priority should be given to primary health care (PHC) linked to essential health services packages, and where they exist, free health-care policies need to be effectively implemented.
Free health-care policies require all countries to progressively increase their investment in health, moving towards allocating at least 15% of their annual budget to health or at least 5% of their annual gross domestic product (GDP) to government health-care expenditure, as appropriate. Ways to increase health budgets may include improving tax collection or initiating social health insurance schemes with everyone receiving services according to their need (See Part 1).
Civil society and community advocacy are essential to support inclusive, effective and transparent financing policies. Advocates can help push decisions and implementations forward through accountability-focused activities and also reduce the risk of corruption.
3: Improve Involvement of CSOs and Citizens, Transparency and Accountability at All Levels
SUMMARY: Civil society is one of three key partners required for effective health governance, alongside the state and health-service providers. The participation of the population, communities and civil society in national health system governance is essential for the system to be responsive, trusted, co-owned by the people and accountable for pursuing equitable progress towards UHC.
According to WHO, effective health governance requires the full engagement of three key stakeholders:
- The State (government organizations and agencies at central and district level)
- Health service providers (public and private, for and not-for-profit, clinical, para-medical and non-clinical health services providers; unions and other professional associations; networks of care)
- The citizen (population representatives, patients’ associations, CSOs, NGOs, citizens associations protecting the poor, grassroots advocates, etc.)
Civil society must be actively engaged at all stages of national policy-making to facilitate community engagement in planning, budgeting, citizen-led monitoring of progress and commitments toward intended UHC outcomes. Strengthening social-led accountability is necessary to maintain the integrity of health systems, prevent corruption-related resource drain, and ensure more accessible, appropriate and sustainable health programs.
Responses to COVID-19
As the COVID-19 pandemic has laid bare the existing state of inequities and the futility of a one-size-fits-all approach, more global and national leaders acknowledge the need for civil society engagement and social participation for health decision-making. Participatory governance is essential to ensure that the rights of vulnerable populations are protected and that they are not unfairly carrying the burden of both increased COVID-19 risks and the negative impacts of restrictions.
Civil society and communities can support governments to conduct a ‘barrier analysis’ to identify the specific types of social, environmental, and institutional gaps that must be addressed to improve access to health within and beyond the COVID-19 pandemic. Governments should also collaborate with civil society to design and implement accountability mechanisms that enable transparent and open communication and respect the ‘right for information’ principle. These accountability mechanisms should monitor the progress of COVID-19 strategies using data disaggregated by gender, age, income, race, ethnicity, migratory status, disability, sexual orientation, gender identity, and geographic location.
At the global stage, the Platform for Community & Civil Society Representatives to the ACT-A is working to ensure communities are heard in every part of the COVID-19 response—across ACT-A’s pillars of diagnostics, therapeutics, vaccines, and health systems. While formal opportunities for engagement with the national COVID-19 response plans have been limited in most countries, CSOs have been active in demanding and ensuring accountability from governments, creating demand for vaccines, and supporting equitable policies.
Countries should ensure civil society has the freedom of association, peaceful assembly, and expression to support social participation and strengthen health systems. Governments should only impose restrictions on these liberties to the minimum extent required to prevent the spread of the COVID-19 virus. They should not continue to use these restrictions beyond what is necessary based on scientific evidence. To ensure restrictions are necessary, proportionate to the risks, and implemented in a non-discriminatory manner, communities must have a role in designing and evaluating policies. Finally, given the disproportionate impact seen so far among women, countries should involve women in decision-making and mainstream a gender perspective in all COVID-19 response and recovery activities.
4: Support Health Workers
SUMMARY: A well trained and resourced multidisciplinary primary health-care team is a critical component of UHC, especially in expanding population coverage at the community level and reaching the last mile.
As the COVID-19 pandemic has shown, without health-care workers, the national health system is meaningless. Having an adequate number of health workers (who are well trained and resourced) is essential to provide services that are tailored to the unique needs of communities, especially those who are currently underserved and vulnerable.
The global health emergency caused by COVID-19 demonstrates the urgency for countries to invest in their health workforce at all levels. Scaled-up investment in the health workforce must include:
- Providing training on infection prevention and control protocols, including appropriate hand hygiene, safe patient management processes in health-care settings, and ensuring compliance is monitored
- Briefing health workers on their rights, roles, responsibilities, and risks
- Ensuring decent working conditions, decent pay, and manageable workloads
- Providing occupational safety to protect workers from infection, such as with personal protective equipment (PPE); access to effective diagnostics, therapeutics, vaccines, continued salary payment during illness; and training on the appropriate use of PPE
- Offering psychosocial support and counselling as well as implementing stress-reduction measures that are appropriate for the context
- Condemning violence and discrimination against health workers, including fear and stigma that they could spread the virus
- Providing training and resources to address health workers’ biases and stigma that can act as barriers to access to health services
- Supporting health programmes to retain their trained frontline staff and continue their salary payments
- Gender-sensitive approaches, given women make up 70% of the global health workforce.
In general, and wherever possible, UHC policies, plans, and reports should include a focus on investment in the health workforce. Frontline health workers are under-resourced and insufficiently trained in some of the diseases and health issues most frequently faced by the poorest and most marginalized groups, such as those living with disability or HIV. Despite this, they play a crucial role in linking these communities to the health system.
It is also critical to ensure that adequate funding is earmarked for the training and capacity-building of both community and frontline health workers. This is necessary to support them in providing inclusive, holistic, and equitable health services, especially to those most marginalized.
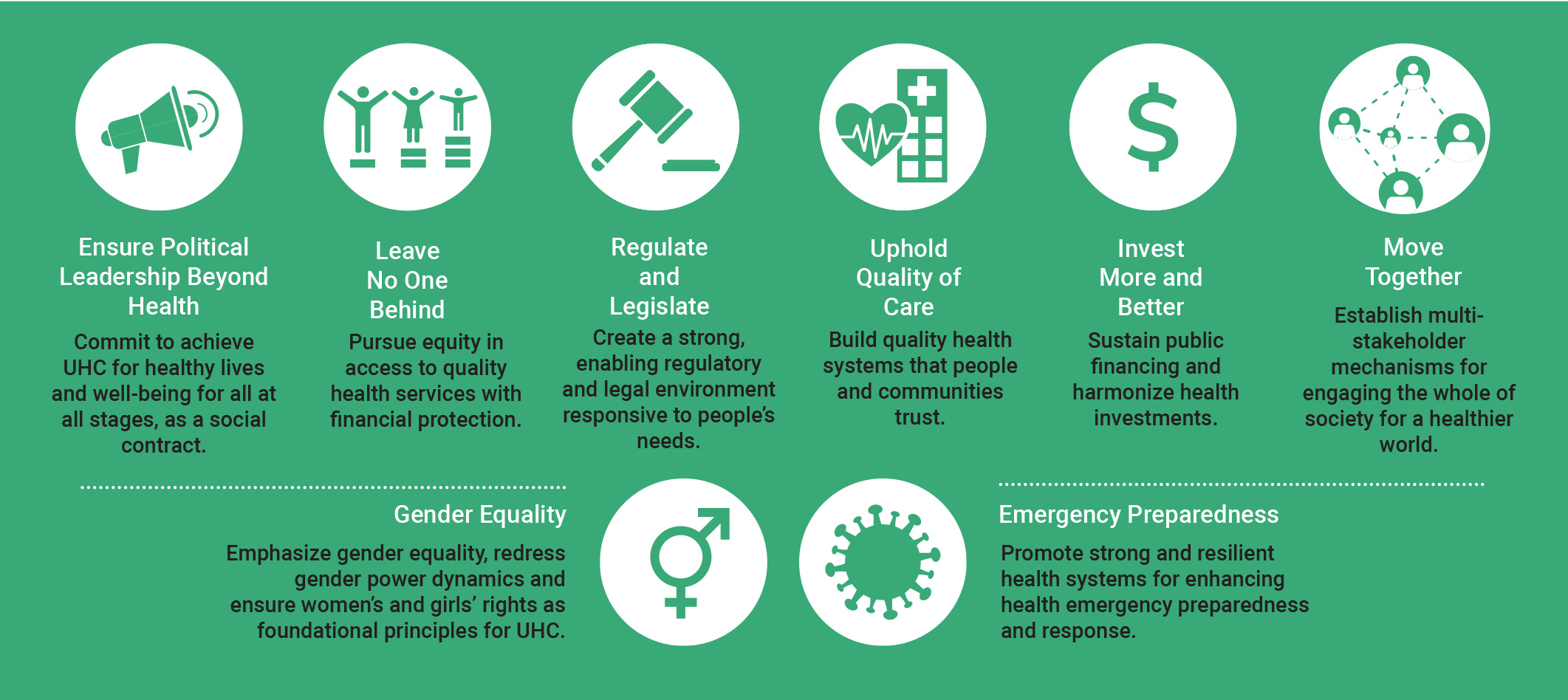
UHC2030 Key Asks
The Key Asks from the UHC Movement are core requests for governments and political leaders to take action on UHC. They were created collectively by a range of health and other stakeholders worldwide, including parliamentarians, civil society, the private sector, agencies, networks, and academia. Developed in the lead up to and during the UHC High-Level Meeting in 2019, the Key Asks continue to provide an important framework for advocacy. In addition to the six initial Key Asks, ‘gender equality’ and ’emergency preparedness’ were later added as cross-cutting asks.
- Ensure Political Leadership Beyond Health
- Leave No One Behind
- Regulate and Legislate
- Uphold Quality of Care
- Invest More, Invest Better
- Move Together
- Gender Equality
- Emergency Preparedness
The key messages from civil society described above complement the Key Asks of the broader UHC movement and highlight civil society perspectives. Learn more about the Key Asks in eight commitment areas: